Best Pericardiocentesis Procedure in Hyderabad
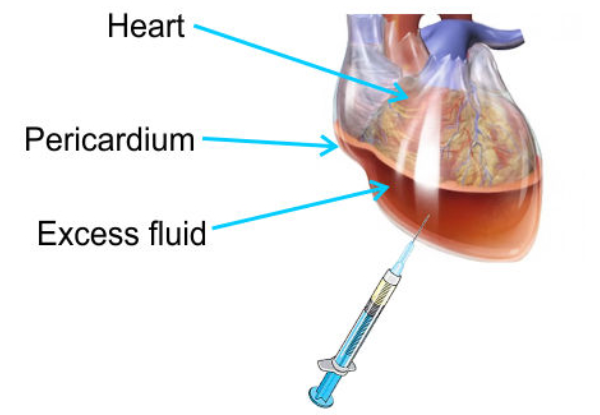
Pericardiocentesis is a medical procedure in which a needle is inserted into the pericardial sac (the lining around the heart) to remove excess fluid that has accumulated within the sac. This excess fluid, called pericardial effusion, can cause pressure on the heart and impair its ability to pump effectively, potentially leading to a life-threatening condition known as cardiac tamponade.
Purpose of Pericardiocentesis
- Relieve Cardiac Tamponade: The primary indication for pericardiocentesis is to treat cardiac tamponade, a condition where the accumulation of fluid in the pericardium puts pressure on the heart, impairing its ability to pump blood properly. This can lead to severe hypotension (low blood pressure), shock, and organ failure if not treated promptly.
- Diagnostic Purposes: In some cases, the procedure is performed to collect a sample of the pericardial fluid for analysis. This helps to identify the underlying cause of the fluid buildup, such as infection, cancer, or autoimmune diseases.
Best Pericardiocentesis Procedure in Hyderabad
Pericardiocentesis is a critical medical procedure in which a needle is carefully inserted into the pericardial sac (the lining around the heart) to remove excess fluid, known as pericardial effusion. This fluid buildup can exert dangerous pressure on the heart and impair its ability to pump effectively, potentially leading to a life-threatening condition called cardiac tamponade.
Purpose of PericardiocentesisRelieve Cardiac Tamponade: The main reason for performing pericardiocentesis is to treat cardiac tamponade. This condition arises when fluid accumulation in the pericardium places pressure on the heart, restricting its function. If untreated, it can result in severe hypotension, shock, and organ failure. The Best Pericardiocentesis Procedure in Hyderabad ensures timely and accurate intervention, often in emergency settings.
Diagnostic Purposes: In addition to being life-saving, the procedure can be used diagnostically. By analyzing the removed fluid, doctors can identify causes such as infections, cancers, or autoimmune disorders, helping guide further treatment.
Indications for Pericardiocentesis
- Cardiac Tamponade: This is the most urgent reason for performing pericardiocentesis. Symptoms of tamponade include low blood pressure, shortness of breath, muffled heart sounds, distended neck veins (jugular venous distention), and pulses paradoxus (a drop in blood pressure during inhalation).
- Pericardial Effusion: Accumulation of fluid in the pericardium, which can be due to several causes, including:
- Infections (e.g., viral, bacterial, tuberculosis).
- Cancer (e.g., metastatic disease).
- Autoimmune conditions (e.g., lupus, rheumatoid arthritis).
- Post-surgical or post-infarction (following heart surgery or a heart attack).
- Trauma or injury to the chest.
- Diagnostic Evaluation: In cases where the cause of the pericardial effusion is unclear, a sample of the pericardial fluid may be collected for analysis (e.g., cell count, culture, cytology, or biochemical testing).
Procedure Overview
Preparation:
- The procedure is usually done in a hospital setting by a cardiologist or a trained healthcare provider.
- The patient is often sedated, and local anesthesia is administered to numb the area where the needle will be inserted.
- The electrocardiogram (ECG) is typically monitored during the procedure to watch for any changes in heart rhythm, as the needle insertion could potentially cause arrhythmias.
Positioning:
- The patient is positioned lying on their back or slightly tilted, depending on the location of the effusion and the approach chosen for the procedure.
- Ultrasound or guidance imaging (such as echocardiography) is often used to identify the pericardial fluid and the safest entry point for the needle.
Needle Insertion:
- A fine needle or catheter is inserted through the skin, typically near the lower part of the sternum or under the ribs.
- Under ultrasound guidance, the needle is carefully advanced toward the pericardial space, avoiding nearby structures like the lungs and major blood vessels.
- Once the needle reaches the pericardium, the fluid is aspirated (removed) and sent for analysis if necessary.
Post-Procedure Monitoring:
- After the procedure, the patient is monitored for complications such as bleeding, infection, or arrhythmias.
- If a large volume of fluid was removed, patients may also need to be monitored for signs of hypotension or re-expansion pulmonary edema, a rare complication where the lung tissue swells after the pericardial pressure is reduced too quickly.
Risks and Complications
Though pericardiocentesis is generally safe, it carries potential risks, including:
- Infection: As with any invasive procedure, there is a risk of introducing an infection. This is minimized with proper sterilization of the procedure site and the use of antibiotics if necessary.
- Bleeding: Accidental injury to nearby structures, such as blood vessels or the heart itself, can cause bleeding. In rare cases, a hematoma (a collection of blood) may form in the pericardial sac.
- Arrhythmias: The insertion of the needle can sometimes irritate the heart, leading to arrhythmias (irregular heartbeats). These are typically transient but may require treatment if they persist.
- Cardiac Injury: Although rare, the needle can puncture the heart or other vital structures, leading to serious complications.
- Pneumothorax: In rare cases, the procedure can cause a pneumothorax (air in the chest cavity), especially if the needle punctures the lung.
- Re-accumulation of Fluid: Sometimes, fluid may begin to accumulate again after the procedure, requiring further interventions such as a pericardial window or a catheter to drain the fluid over time.
- Re-expansion Pulmonary Edema: If a large amount of fluid is removed too quickly, it can cause re-expansion pulmonary edema, which is swelling of the lungs due to a sudden drop in pressure around the heart.
Post-Procedure Care
- Observation: The patient is typically monitored for a few hours after the procedure to ensure there are no immediate complications.
- Follow-up Imaging: In some cases, follow-up echocardiograms or chest X-rays may be performed to ensure that the fluid does not return or that no complications, such as bleeding or pneumothorax, occur.
- Medications: Depending on the underlying cause of the pericardial effusion, medications may be prescribed (e.g., antibiotics for infection, chemotherapy for cancer, or anti-inflammatory drugs for autoimmune diseases).
Alternative Procedures
In cases where pericardiocentesis is not sufficient or appropriate, or when the fluid re-accumulates, alternative interventions may include:
- Pericardial Window: A surgical procedure in which a small portion of the pericardium is removed to allow for continuous drainage of fluid. This is typically done if there are concerns about recurrent effusions or if a catheter needs to be left in place.
- Pericardial Catheter Drainage: A catheter can be placed in the pericardial sac to drain fluid over a longer period of time. This is used in cases of recurrent pericardial effusion or when the underlying cause of fluid buildup persists.
Conclusion
Pericardiocentesis is an essential procedure for managing pericardial effusion, especially in the setting of cardiac tamponade, where excess fluid compresses the heart and impairs its function. It helps relieve pressure on the heart, restore normal circulation, and can provide valuable diagnostic information regarding the cause of the effusion.
Explore More : Cardiac Catheterization Treatment in Hyderabad
